Unlocking Potential: The Role of Testosterone Therapy in Fertility
In the intricate tapestry of human reproduction, hormones play a pivotal role, weaving together various threads of health, desire, and the ability to conceive. Among these hormones, testosterone has often been cast in the spotlight, primarily associated with masculinity and vitality. However, as research delves deeper into the complexities of male fertility, testosterone therapy has emerged as a compelling topic of discussion. This article navigates the nuanced intersection of testosterone therapy and fertility, exploring how this treatment may offer hope to those on their journey to parenthood. By illuminating both the scientific underpinnings and the implications for aspiring fathers, we aim to provide a comprehensive perspective on a subject that is reshaping the conversation around fertility in the modern age.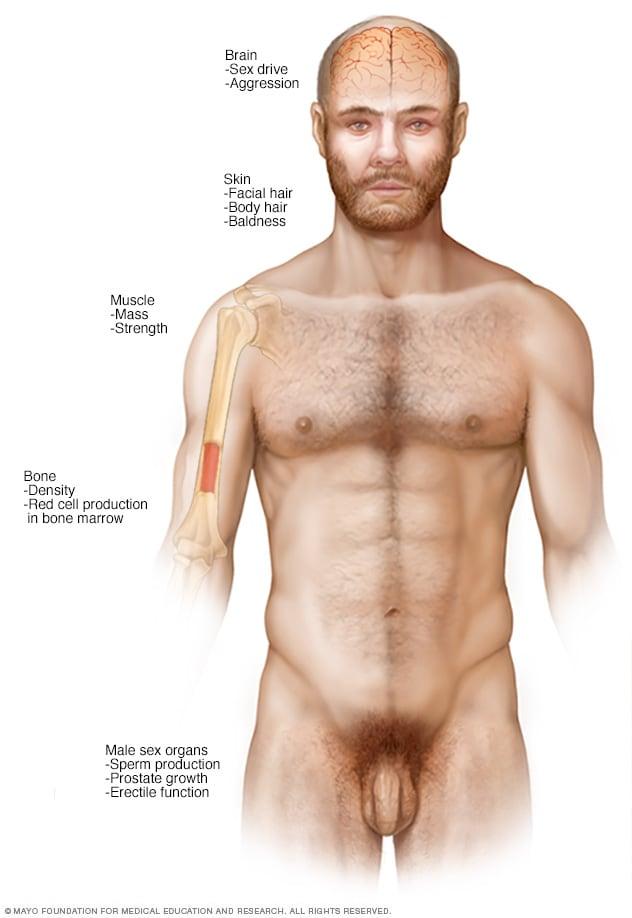
Understanding the Role of Testosterone in Male Fertility
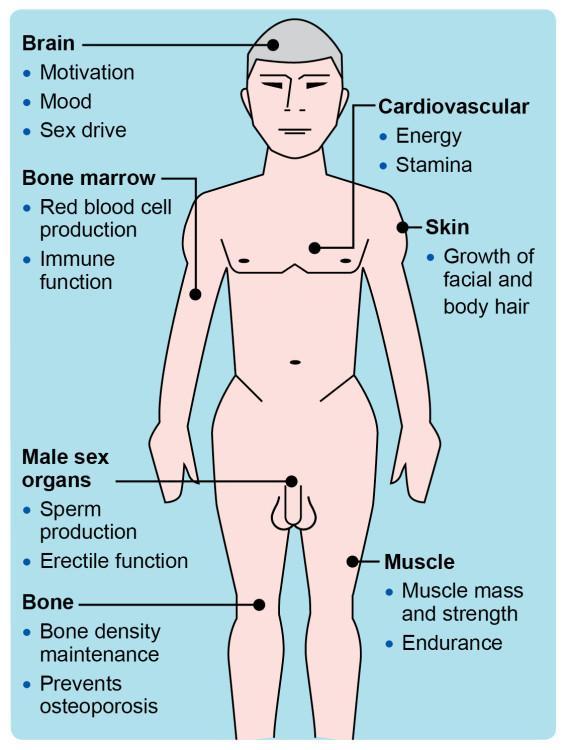
Testosterone is a vital hormone that plays a significant role in various physiological processes in men, with one of its key functions being the regulation of fertility. This hormone influences several aspects of reproductive health, including sperm production, libido, and the overall functioning of the reproductive system. Adequate levels of testosterone are necessary for the proper development of sperm cells in the testes, known as spermatogenesis. When testosterone levels fall below normal, men may experience reduced sperm quality and quantity, leading to difficulties in achieving conception.
In the context of fertility treatment, testosterone therapy can be a double-edged sword. While it can help elevate testosterone levels and improve symptoms associated with low testosterone, such as fatigue and loss of libido, it may also have negative effects on fertility. Exogenous testosterone can suppress the body’s natural testosterone production and result in decreased stimulation of the testicles, inhibiting spermatogenesis. Therefore, it is crucial for men considering testosterone therapy to have a thorough discussion with their healthcare provider to weigh the potential benefits against the possible implications for their fertility.

Assessing the Need for Testosterone Therapy in Fertility Challenges
When exploring the role of testosterone therapy in addressing fertility challenges, it’s essential to evaluate various factors that can contribute to a man’s reproductive health. Hormonal imbalances can significantly affect sperm production and quality, and testosterone plays a crucial role in this process. Some key indicators for assessing the need for testosterone therapy include:
- Low testosterone levels: Measured through blood tests, levels below the normal range may require further evaluation.
- Symptoms of hypogonadism: These may include fatigue, decreased libido, mood changes, and difficulty concentrating.
- Previous fertility results: A history of low sperm counts or poor sperm motility can underscore the importance of hormone assessment.
Additionally, the decision to embark on testosterone therapy must be approached with caution, as it can have implications for overall health and fertility outcomes. It is vital to differentiate between primary and secondary hypogonadism, as treatment protocols may vary. A tailored approach should consider the following factors before making a therapeutic decision:
| Consideration | Implications for Therapy |
|---|---|
| Age | Older men may have different therapy needs. |
| Underlying health conditions | Conditions like diabetes can affect testosterone levels. |
| Personal and family history | Genetic factors may influence treatment options. |
Exploring the Benefits and Risks of Hormone Replacement
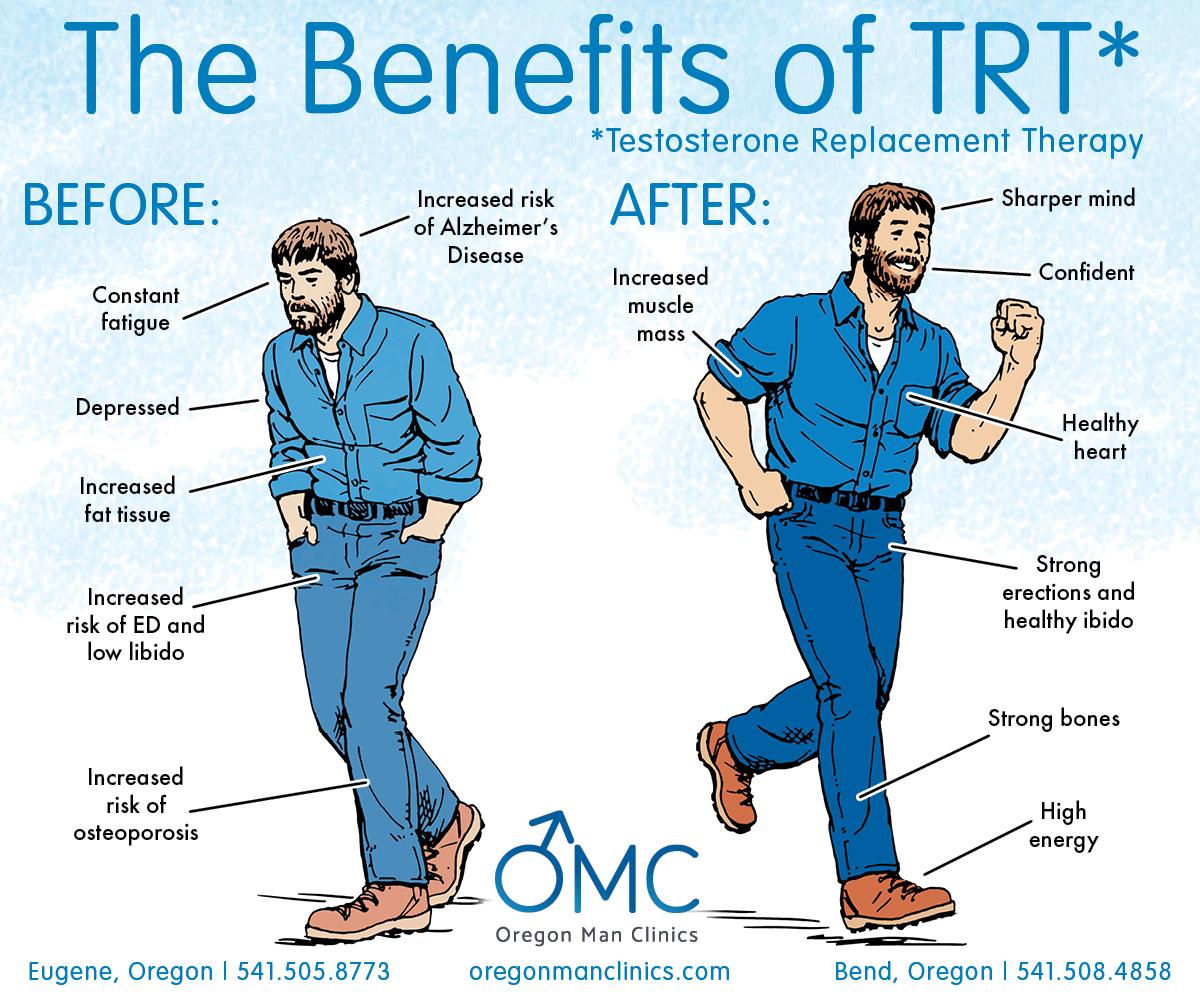
Hormone replacement therapy (HRT), particularly testosterone therapy, has gained attention for its potential benefits in enhancing fertility among men experiencing hormonal imbalances. Some of the notable advantages include:
- Improved Sperm Production: Testosterone plays a critical role in spermatogenesis, and therapy may boost sperm count and motility.
- Enhanced Libido: Increased testosterone levels can improve sexual desire, which may lead to a higher likelihood of conception.
- Better Mood and Energy Levels: Restoring hormonal balance can positively influence mental health and physical stamina, fostering a conducive environment for starting a family.
However, there are notable risks associated with HRT that should not be overlooked. These include:
- Potential for Infertility: Ironically, while testosterone therapy can enhance fertility for some, it may also lead to reduced natural testosterone production, decreasing sperm production over time.
- Cardiovascular Issues: There are concerns that testosterone therapy may increase the risk of heart problems, particularly in older men or those with preexisting conditions.
- Hormonal Imbalances: Mismanagement of testosterone levels can lead to complications, including estrogen dominance and mood swings.
| Considerations | Benefits | Risks |
|---|---|---|
| Testosterone Therapy | Increased sperm production, enhanced libido | Potential for infertility, cardiovascular issues |
| Hormonal Balance | Better mood and energy | Hormonal imbalances |
Tailoring Treatment: Finding the Right Dosage and Method
The effectiveness of testosterone therapy for fertility largely hinges on personalized treatment approaches that consider individual hormonal needs, lifestyle factors, and underlying health conditions. To achieve a positive outcome, healthcare professionals typically assess various factors, such as:
- Age: Younger patients may require different dosages compared to older individuals.
- Baseline hormone levels: Initial testosterone levels can guide dosage adjustments.
- Duration of treatment: Long-term therapy might necessitate a reevaluation of dosage.
Determining the appropriate delivery method—be it injections, gels, or patches—is crucial for optimizing results. Each method has its own set of advantages and drawbacks. For instance:
| Delivery Method | Advantages | Drawbacks |
|---|---|---|
| Injections | Quick absorption and higher efficacy | Requires frequent visits to healthcare provider |
| Gels | Convenient and easy to use | Risk of transfer to others |
| Patches | Steady hormonal release | Skin irritation may occur |
By tailoring both dosage and delivery method, individuals on testosterone therapy can enhance their fertility potential while minimizing side effects, ensuring a smoother path toward achieving their reproductive goals.
Integrating Testosterone Therapy with Other Fertility Treatments
When considering testosterone therapy for individuals facing fertility issues, it is essential to understand how to effectively integrate it with other fertility treatments. Testosterone therapy can enhance hormonal balance and improve sperm production, but it often works best in conjunction with additional therapeutic approaches. Below are strategies to ensure a more comprehensive treatment plan:
- Comprehensive Hormonal Assessment: Prior to starting testosterone therapy, it’s crucial to evaluate all hormones involved in reproductive health, including LH, FSH, and estradiol.
- Combining With Assisted Reproductive Technologies (ART): Testosterone therapy can be paired with procedures such as IVF or IUI to increase the chances of successful conception.
- Monitoring Progress: Regular testing of testosterone levels and sperm analysis can guide adjustments in therapy, optimizing the fertility treatment outcome.
Another aspect to consider is the timing and dosage of testosterone therapy in relation to fertility cycles. Proper synchronization can maximize therapeutic benefits and increase the likelihood of conception. Below is a simplified table indicating the potential benefits and considerations when combining testosterone therapy with other treatments:
| Integration Strategy | Potential Benefits |
|---|---|
| Combined with Clomiphene Citrate | Enhanced sperm production |
| Before Sperm Retrieval | Increased testosterone levels for optimal quality |
| Post-Therapy Recovery | Improved hormonal balance for long-term fertility |
Lifestyle Factors Influencing Testosterone Levels and Fertility
Understanding the intricate relationship between lifestyle choices and testosterone levels is essential, especially for those exploring fertility options. Diet and nutrition play a pivotal role; a balanced intake of macronutrients—especially proteins, healthy fats, and carbohydrates—can enhance hormonal balance. Foods rich in vitamins and minerals such as zinc, vitamin D, and omega-3 fatty acids significantly support testosterone production. Additional lifestyle factors include physical activity and sleep quality; regular exercise, particularly resistance training, has been proven to increase testosterone levels, while adequate sleep regulates hormone secretion.
Moreover, environmental factors and emotional well-being should not be overlooked. Stress management is vital; chronic stress elevates cortisol levels, which inversely affect testosterone. Avoiding exposure to endocrine disruptors found in plastics, chemicals, and certain pesticides can also help maintain hormonal health. The following table highlights key lifestyle factors and their influence on testosterone levels:
| Factor | Impact on Testosterone |
|---|---|
| Balanced Diet | Boosts testosterone and overall hormonal health |
| Regular Exercise | Increases levels through improved metabolic health |
| Sufficient Sleep | Regulates hormone production and balance |
| Stress Management | Reduces cortisol and supports testosterone levels |
| Avoiding Endocrine Disruptors | Prevents negative impacts on hormonal balance |
Future Directions in Research on Testosterone and Reproductive Health
The evolving landscape of testosterone therapy presents a myriad of opportunities for advancing our understanding of its role in reproductive health. As researchers delve deeper, it is crucial to investigate how varying doses and formulations of testosterone can affect male fertility. Current studies suggest a complex interplay between testosterone levels and sperm production, emphasizing the need for optimizing treatment regimens tailored to individual patient profiles. Future research should focus on potential biomarkers that predict the response to therapy, which could lead to personalized approaches in managing infertility linked to low testosterone levels.
Moreover, interdisciplinary collaboration will be vital in uncovering the long-term effects of testosterone therapy on reproductive health. This can include insights from endocrinologists, reproductive specialists, and urologists to create comprehensive treatment frameworks. Future studies might explore the following areas:
- Impact of testosterone therapy on sexual function
- Role of lifestyle factors in moderating outcomes
- Effects on partner fertility
- Comparative analysis of various formulations
Additionally, long-term cohort studies could provide invaluable data on the sustainability of fertility post-therapy cessation, clarifying the balance between hormonal replacement and reproductive health. Addressing these questions will pave the way for innovative treatment paradigms that not only aim to restore testosterone levels but also enhance overall fertility outcomes.
Q&A
Q&A: Understanding Testosterone Therapy for Fertility
Q1: What is testosterone therapy and how does it relate to fertility?
A1: Testosterone therapy involves the administration of testosterone to individuals with low hormone levels. While primarily known for its role in enhancing libido and muscle mass, recent studies have explored its potential implications for male fertility. Adequate testosterone levels are crucial for the proper functioning of the male reproductive system, including sperm production, which makes understanding its impact on fertility essential.
Q2: Can testosterone therapy actually improve sperm production?
A2: It might seem paradoxical, but testosterone therapy can sometimes suppress sperm production in men undergoing treatment for low testosterone. This is because external testosterone can inhibit the natural hormone signals that stimulate spermatogenesis. However, in certain cases of hypogonadism where low testosterone is the primary issue hindering fertility, appropriate management can potentially restore hormone balance and improve sperm output.
Q3: Who should consider testosterone therapy for fertility purposes?
A3: Men experiencing difficulties with fertility who also show signs of low testosterone levels might benefit from this therapy. It’s crucial to undergo a comprehensive evaluation from a healthcare professional, who can determine if underlying hormonal imbalances are contributing to fertility issues. Individual cases vary widely, so personal consultation is key.
Q4: What are the risks associated with testosterone therapy?
A4: Like any medical treatment, testosterone therapy comes with potential risks. These can include the exacerbation of sleep apnea, increased red blood cell counts, and potential cardiovascular concerns. Most importantly for fertility, therapy can lead to reduced sperm production in some men due to disturbed hormonal regulation. Thorough discussions with a qualified healthcare provider can help weigh the benefits against these risks.
Q5: Are there alternatives to testosterone therapy for improving fertility?
A5: Yes, there are several alternatives available. Lifestyle changes such as diet, exercise, and maintaining a healthy weight can significantly impact testosterone levels and overall fertility. Additionally, certain medications or treatments that directly target hormonal imbalances or address underlying issues (like varicocele repair) can be more effective for enhancing fertility.
Q6: How can men prepare for discussions about testosterone therapy with their doctors?
A6: Preparing for a consultation involves being well-informed and ready to discuss personal health history, symptoms, and any previous fertility treatments. Keeping a record of lifestyle factors—like diet, exercise, and stress—can provide valuable insights for the doctor. Asking specific questions about the potential benefits and side effects of testosterone therapy can lead to a more productive dialogue.
Q7: Is there ongoing research related to testosterone therapy and its effects on fertility?
A7: Absolutely! The field of reproductive health is dynamic, with ongoing research aimed at untangling the complexities of hormone therapy and fertility. Studies are investigating how testosterone levels influence sperm health, alternative therapeutic methods, and the long-term effects of therapy on male reproductive health. Staying abreast of new findings can be beneficial for those considering this path.
Q8: What should men take away from this discussion about testosterone therapy and fertility?
A8: The relationship between testosterone and fertility is multifaceted and requires careful navigation. While testosterone therapy has a role in treating certain hormonal deficiencies, it is not a one-size-fits-all solution for fertility issues. Open communication with healthcare providers and consideration of individual circumstances are vital steps in making informed decisions about treatment options. Always remember, personal health and fertility journeys are best approached with a tailored strategy!
To Wrap It Up
As we draw the curtain on our exploration of testosterone therapy and its implications for fertility, it becomes clear that this topic weaves a complex tapestry of science, hope, and individual experience. While testosterone therapy may emerge as a beacon of possibility for some, it is paramount to navigate this journey with informed guidance, considering both the potential benefits and the nuances of hormonal balance.
Acknowledging the myriad factors that influence fertility, it’s essential to approach testosterone therapy within the broader context of reproductive health. Each individual’s path is unique, shaped by personal circumstances and medical history. Consultation with healthcare professionals remains crucial to tailor a strategy that aligns with one’s aspirations and well-being.
As we step into the future of fertility treatments, let us embrace a spirit of curiosity and collaboration, seeking knowledge and support as we explore the myriad ways to nurture life. In this evolving landscape, the quest for parenthood continues to inspire innovation and understanding, reminding us that hope springs eternal, grounded in science and nurtured by community.










