In the complex landscape of post-cancer recovery, where healing takes on many forms, the conversation around hormonal health has emerged as a pivotal topic for many survivors. Among the myriad of treatment options, testosterone therapy is gaining attention for its potential to restore vitality and improve quality of life following cancer treatment. For those navigating the often turbulent waters of side effects and emotional shifts, understanding the role of testosterone becomes crucial. This article delves into the nuances of testosterone therapy after cancer treatment, exploring the scientific underpinnings, potential benefits, and necessary considerations that can empower survivors to reclaim their health and wellness in a post-cancer world. Join us as we unpack this multifaceted topic, shedding light on a therapy that may offer not just physical recovery but a renewed sense of identity and strength.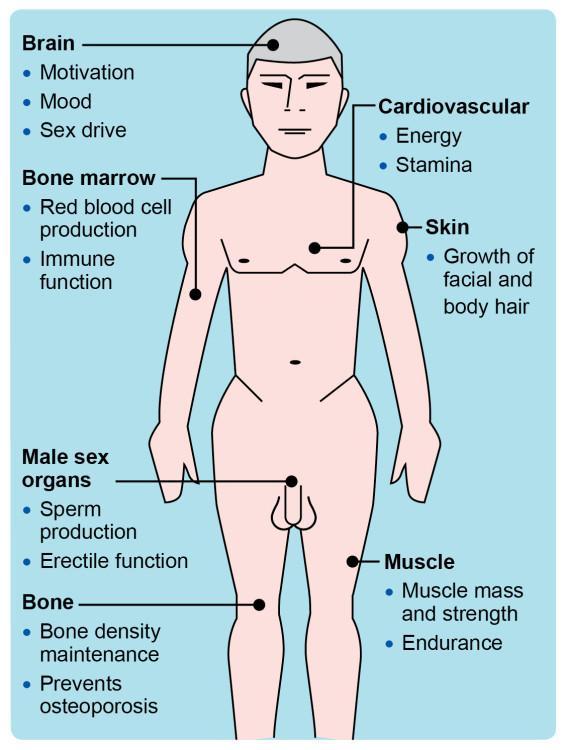
Understanding the Role of Testosterone in Post-Cancer Recovery
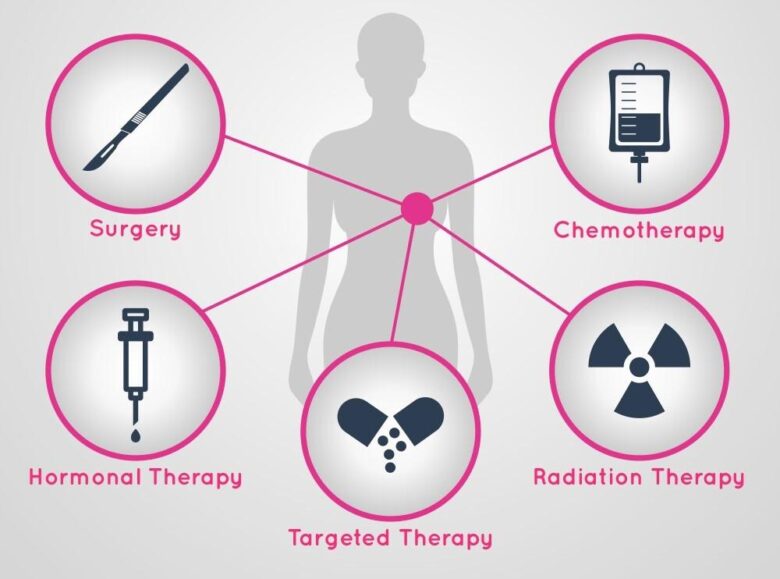
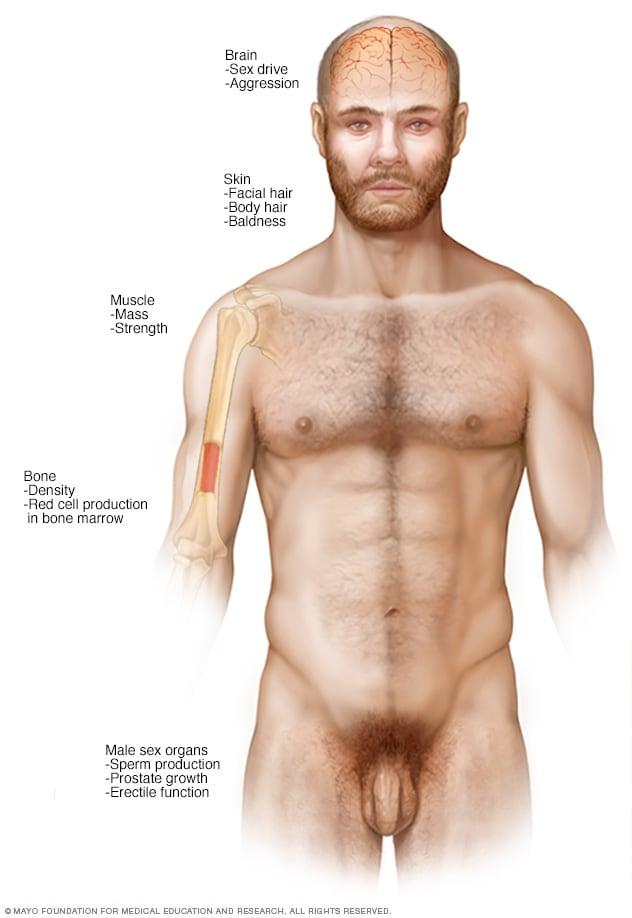
Testosterone plays a crucial role in the physical and mental well-being of individuals, particularly after undergoing cancer treatment. For many survivors, the impacts of cancer and its treatments—such as chemotherapy and radiation—can lead to hormonal imbalances, including low testosterone levels. This deficiency might manifest as fatigue, reduced muscle mass, and diminished libido, greatly affecting a person’s quality of life. Understanding how testosterone contributes to recovery is vital; it not only aids in rebuilding muscle and stamina but also supports mood regulation and cognitive function, allowing survivors to regain a sense of normalcy.
Incorporating testosterone therapy post-cancer can be a pivotal step in the recovery journey. Benefits of testosterone therapy include:
- Increased Energy Levels: Helps counteract the fatigue often experienced after treatment.
- Improved Muscle Strength: Supports physical rehabilitation and enhances overall fitness.
- Enhanced Mood and Mental Clarity: Aids in alleviating depression and cognitive fog.
- Boosted Libido: Addresses issues relating to sexual health and intimacy, often affected post-treatment.
However, it is essential for survivors to consult healthcare professionals to tailor therapy to their specific needs. Proper monitoring and adjustments can ensure optimal results, minimizing potential side effects. Regular follow-ups and blood tests are crucial in assessing the effectiveness of the treatment and making necessary changes.
Navigating the Emotional and Physical Impact of Hormonal Changes
Hormonal changes can create a ripple effect in both emotional and physical well-being, particularly for individuals undergoing testosterone therapy following cancer treatment. Understanding these fluctuations is critical for managing your health effectively. Patients often experience a range of emotions, from anxiety and mood swings to increased feelings of irritability. Addressing these emotional challenges is vital, and may include strategies such as:
- Open conversations with health professionals about emotional symptoms
- Support groups to share experiences with others
- Mindfulness practices to cultivate emotional resilience
On the physical side, testosterone therapy can lead to noticeable changes in energy levels, libido, and overall physical health. As the body adjusts to new hormone levels, patients may encounter symptoms like fatigue or weight fluctuations. Monitoring these changes is essential; a proactive approach can help in recognizing shifts promptly. To support physical wellness during this transition, consider incorporating:
| Wellness Strategies | Description |
|---|---|
| Regular Exercise | Boosts mood and energy levels |
| Balanced Nutrition | Supports overall health and hormone balance |
| Sufficient Sleep | Enhances recovery and emotional stability |
Evaluating When Testosterone Therapy is Appropriate for Survivors
For many cancer survivors, navigating the aftermath of treatment can be just as challenging as the diagnosis itself. In some cases, deficiencies in testosterone levels may arise as a consequence of certain cancer treatments, particularly those involving chemotherapy or radiation. Assessing the necessity of testosterone therapy involves considering a blend of physical symptoms and overall health profiles. Symptoms to watch out for include:
- Fatigue
- Reduced libido
- Loss of muscle mass
- Depression or mood changes
It is essential for survivors to engage in comprehensive discussions with their healthcare providers. These conversations should include evaluations of blood testosterone levels, an assessment of potential side effects, and a close examination of the survivor’s individual medical history. Risks versus benefits must be weighed carefully; side effects can include:
- Increased risk of cardiovascular issues
- Potential aggravation of prostate problems
- Changes in sleep patterns
| Benefit of Therapy | Considerations |
|---|---|
| Improved energy levels | Regular monitoring needed |
| Enhanced mood stability | Watch for aggravation of anxiety |
| Increased libido and sexual function | Interaction with other medications |

Potential Benefits of Testosterone Therapy for Quality of Life
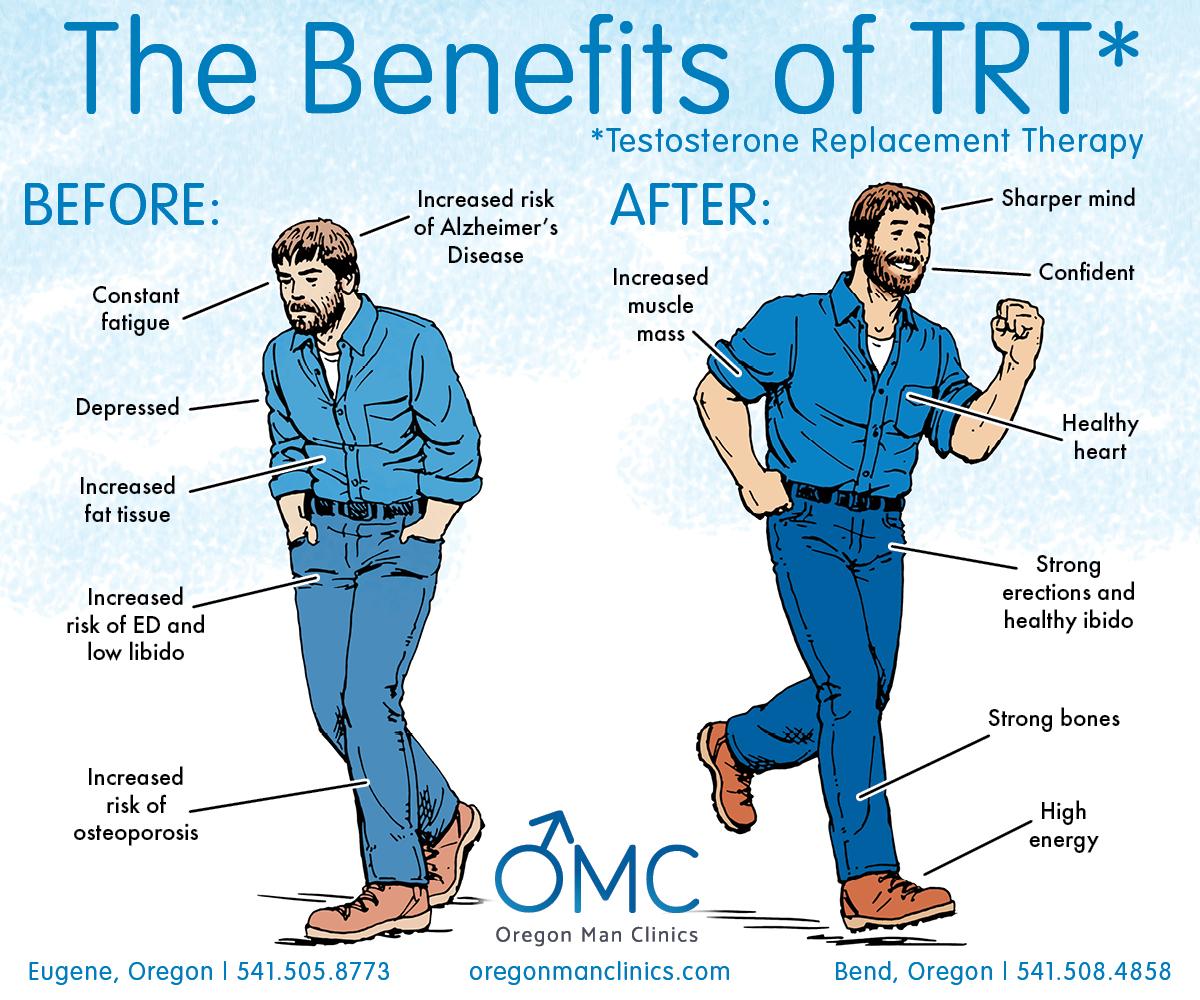
Testosterone therapy can play a pivotal role in enhancing overall well-being for individuals who have undergone cancer treatment. Many survivors experience a range of symptoms stemming from hormonal imbalances, which can significantly affect their quality of life. By restoring testosterone levels, therapy may help alleviate symptoms such as fatigue, depression, and loss of libido, thereby improving emotional and physical well-being. Some potential benefits include:
- Increased Energy Levels: Many patients report feeling more energized and motivated.
- Improved Mood: Testosterone therapy can lead to a more balanced emotional state, decreasing feelings of anxiety and depression.
- Enhanced Cognitive Function: Better concentration and memory are frequently observed.
- Improved Physical Strength: Increased testosterone can facilitate muscle growth and improve overall physical capability.
Moreover, the advantages of testosterone therapy extend beyond mere physical changes. They contribute significantly to enhancing the quality of life for cancer survivors by fostering a sense of normalcy and vitality. It is important to note that the therapy should be tailored to individual needs, considering factors such as age, health status, and previous treatment history. A comprehensive approach may lead to a more fulfilling existence post-treatment. Below is a comparison of life quality indicators before and after testosterone therapy:
| Quality Indicator | Before Therapy | After Therapy |
|---|---|---|
| Energy Levels | Low | Moderate to High |
| Mood | Increased Anxiety | More Stable |
| Physical Strength | Decreased | Increased |
| Cognitive Function | Impaired | Improved |
Risks and Considerations: Ensuring Safe Hormonal Treatment
When considering testosterone therapy after cancer treatment, it’s crucial to assess the potential risks and benefits with meticulous attention. Patients should consult with their healthcare providers to understand how hormone therapy might interact with their medical history and current health status. Factors such as age, type of cancer, and previous treatments play pivotal roles in shaping a tailored approach to therapy. Here are some risks to keep in mind:
- Hormonal Fluctuations: Adjusting testosterone levels can lead to unexpected shifts in mood and energy.
- Cardiovascular Issues: Increased testosterone may elevate the risk of heart-related complications, especially in those with pre-existing conditions.
- Impact on Cancer Recurrence: It’s vital to consider how testosterone could influence the likelihood of cancer returning, particularly in hormone-sensitive cancers.
Monitoring is essential to mitigate potential complications. Regular follow-ups and blood tests allow for real-time adjustments to therapy, ensuring safety and efficacy. Patients should be vigilant about recognizing symptoms that might indicate adverse reactions, including swelling in the legs, shortness of breath, or unusual weight gain. An effective management plan should include:
| Monitoring Aspect | Frequency |
|---|---|
| Blood Tests | Every 3 months |
| Cardiovascular Health Screening | Every 6 months |
| Symptom Assessment | Ongoing |
Tailoring Treatment Plans: Individualized Approaches for Survivors
With the journey of cancer treatment behind them, many survivors face a new set of challenges, including hormonal imbalances that may arise from their therapies. Tailoring treatment plans for these individuals often involves a careful evaluation of their unique circumstances, as testosterone therapy can play a pivotal role in supporting overall well-being. The process requires detailed assessments of physical health, emotional resilience, and lifestyle factors, allowing healthcare providers to pinpoint specific needs and preferences of each survivor.
When considering testosterone therapy, it is crucial to adopt a comprehensive, individualized approach that reflects the survivor’s health goals. This can entail:
- Regular Monitoring: Frequent assessments ensure that hormone levels are within optimal ranges, minimizing potential side effects.
- Patient Input: Involving survivors in treatment decisions helps align therapy with personal aspirations and lifestyle choices.
- Holistic Support: Recommendations for diet, exercise, and mental health can significantly enhance the effectiveness of testosterone therapy.
To better illustrate the components of an individualized treatment plan, the following table summarizes key factors affecting testosterone therapy in cancer survivors:
| Factor | Considerations |
|---|---|
| Age | Age-related hormonal decline may impact therapy decisions. |
| Type of Cancer | Specific cancers may influence the safety and timing of therapy. |
| Emotional Health | Support for anxiety or depression is vital during recovery. |
| Comorbid Conditions | Existing health issues must be managed alongside hormone treatments. |
Building a Supportive Environment for Successful Hormonal Balance
Creating a nurturing atmosphere is paramount for individuals seeking to restore hormonal equilibrium post-cancer treatment. It begins with cultivating a healthy lifestyle that supports overall well-being. This can be achieved through small but impactful changes such as:
- Balanced Nutrition: A diet rich in whole foods, lean proteins, and healthy fats can enhance body function.
- Regular Exercise: Engaging in physical activity, tailored to individual capabilities, can improve mood and metabolic health.
- Sleep Hygiene: Prioritizing quality sleep can significantly affect hormonal levels.
Furthermore, mental and emotional health plays a critical role in the recovery process. Building a support network that includes friends, family, and healthcare professionals ensures that individuals don’t navigate their journey alone. Techniques such as:
- Meditation: Can foster a sense of calm and reduce stress.
- Group Therapy: Provides a platform for sharing experiences and strategies.
- Mindfulness Practices: Help individuals stay grounded and centered.
Q&A
Q&A: Testosterone Therapy After Cancer Treatment
Q1: What is testosterone therapy, and why might it be recommended after cancer treatment?
A1: Testosterone therapy involves the administration of testosterone, a hormone critical for many bodily functions, particularly in men. After cancer treatment, particularly for conditions like prostate cancer, patients may experience low testosterone levels due to hormonal shifts, treatment effects, or removal of hormone-producing organs. This therapy may be recommended to alleviate symptoms such as fatigue, decreased libido, and mood disturbances and to improve the overall quality of life.
Q2: Are there specific types of cancer treatment that can lead to decreased testosterone levels?
A2: Yes, certain treatments can directly impact testosterone production. For instance, surgery that involves removal of the testicles or other hormonal therapies used to treat prostate cancer can lead to lower testosterone levels. Additionally, chemotherapy and radiation therapy, while often effective in targeting cancer cells, can also disrupt the endocrine system, affecting hormone levels including testosterone.
Q3: What potential benefits can testosterone therapy provide to cancer survivors?
A3: For cancer survivors facing low testosterone levels, the potential benefits of therapy include increased energy levels, improved mood and mental clarity, enhanced libido, and better muscle mass and bone density. Patients may also experience improvements in their overall quality of life, which can be particularly important during recovery after cancer treatment.
Q4: Are there any risks associated with testosterone therapy for cancer survivors?
A4: Yes, while testosterone therapy can offer significant benefits, there are potential risks, especially for those with a history of hormone-sensitive cancers, such as prostate cancer. It may exacerbate certain health issues, including cardiovascular problems or potentially stimulate cancer growth. Therefore, careful evaluation and ongoing monitoring by a healthcare professional are essential to ensure that the risks are managed and minimized.
Q5: How do doctors determine if a cancer survivor is a candidate for testosterone therapy?
A5: Doctors typically conduct a thorough evaluation that includes a review of the patient’s medical history, current symptoms, and hormone levels through blood tests. They will assess the type of cancer, its treatment history, and any ongoing risks. A multidisciplinary approach involving oncologists and endocrinologists ensures that the therapy is tailored to each individual’s unique circumstances.
Q6: What should patients consider before starting testosterone therapy?
A6: Patients should engage in open dialogue with their healthcare team. Key considerations include understanding the potential benefits and risks, discussing symptoms they wish to address, and exploring any underlying health concerns. Patients should also reflect on their overall health goals and ensure they have a supportive plan that includes regular follow-up appointments to monitor their progress and adjustment to therapy.
Q7: Is testosterone therapy a lifelong commitment for cancer survivors?
A7: Not necessarily. The duration of testosterone therapy varies among individuals. Some may require long-term therapy to manage ongoing symptoms, while others might find that their testosterone levels stabilize and they can reduce or discontinue treatment. Regular monitoring and assessment by healthcare professionals will guide this decision-making process.
Q8: Where can cancer survivors find more information on testosterone therapy?
A8: Cancer survivors can consult their oncologist or endocrinologist for personalized guidance. Additionally, reputable organizations like the American Cancer Society or the Endocrine Society provide resources and research on hormone therapy. Support groups and forums are also helpful for sharing experiences and insights with others facing similar challenges.
This Q&A format serves to inform cancer survivors about the essential aspects of testosterone therapy post-treatment while addressing concerns and fostering a comprehensive understanding of options available for improving quality of life.
The Conclusion
navigating the journey of recovery after cancer treatment is a complex and deeply personal experience. For many, the struggle with hormonal changes, particularly the decline in testosterone levels, can be a lingering challenge that significantly impacts quality of life. Testosterone therapy presents a potential avenue for those seeking to restore their hormonal balance and regain their vitality.
As we’ve explored, this therapy can offer benefits beyond physical well-being, encompassing emotional resilience and mental clarity. However, it is crucial for survivors to approach this option with careful consideration and professional guidance. Open dialogues with healthcare providers, informed decision-making, and individual treatment plans can pave the way toward a renewed sense of self.
Ultimately, every survivor’s path is unique, and what works for one person may not work for another. As research continues to evolve, the hope is that survivors will find greater support and understanding in their quest for recovery. Embracing the journey ahead, armed with knowledge and the right resources, can lead to renewed possibilities and a brighter, more empowered future after cancer.