Navigating the Balance: An Introduction to Testosterone Therapy Dosage Guidelines
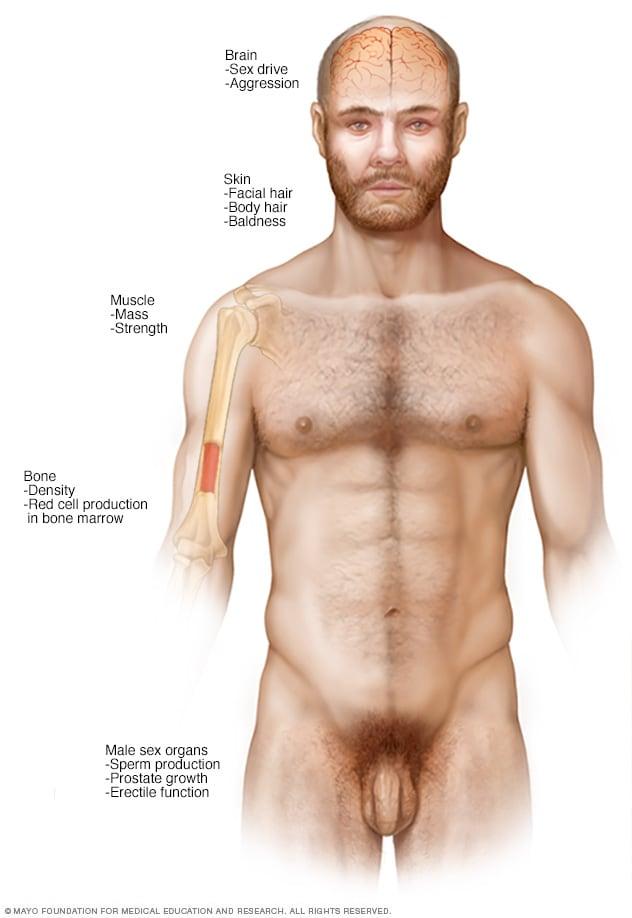
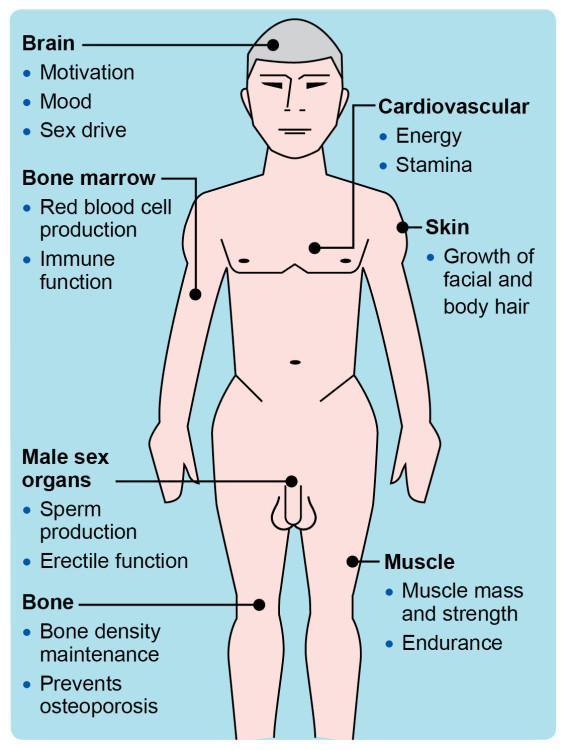
In the realm of hormonal health, testosterone plays a pivotal role, influencing everything from energy levels and muscle mass to mood and libido. As awareness surrounding testosterone therapy grows, so too does the complexity of determining the proper dosage for each individual. With an increasing number of men and women seeking relief from symptoms associated with low testosterone levels, understanding the intricacies of dosage guidelines becomes paramount. This article delves into the essential principles of testosterone therapy, addressing the various factors that influence dosage recommendations, the importance of individualized treatment, and the latest evidence-based practices that can guide both healthcare providers and patients in this delicate balancing act. Join us as we explore the nuances of optimal testosterone therapy, paving the way for informed choices and improved well-being.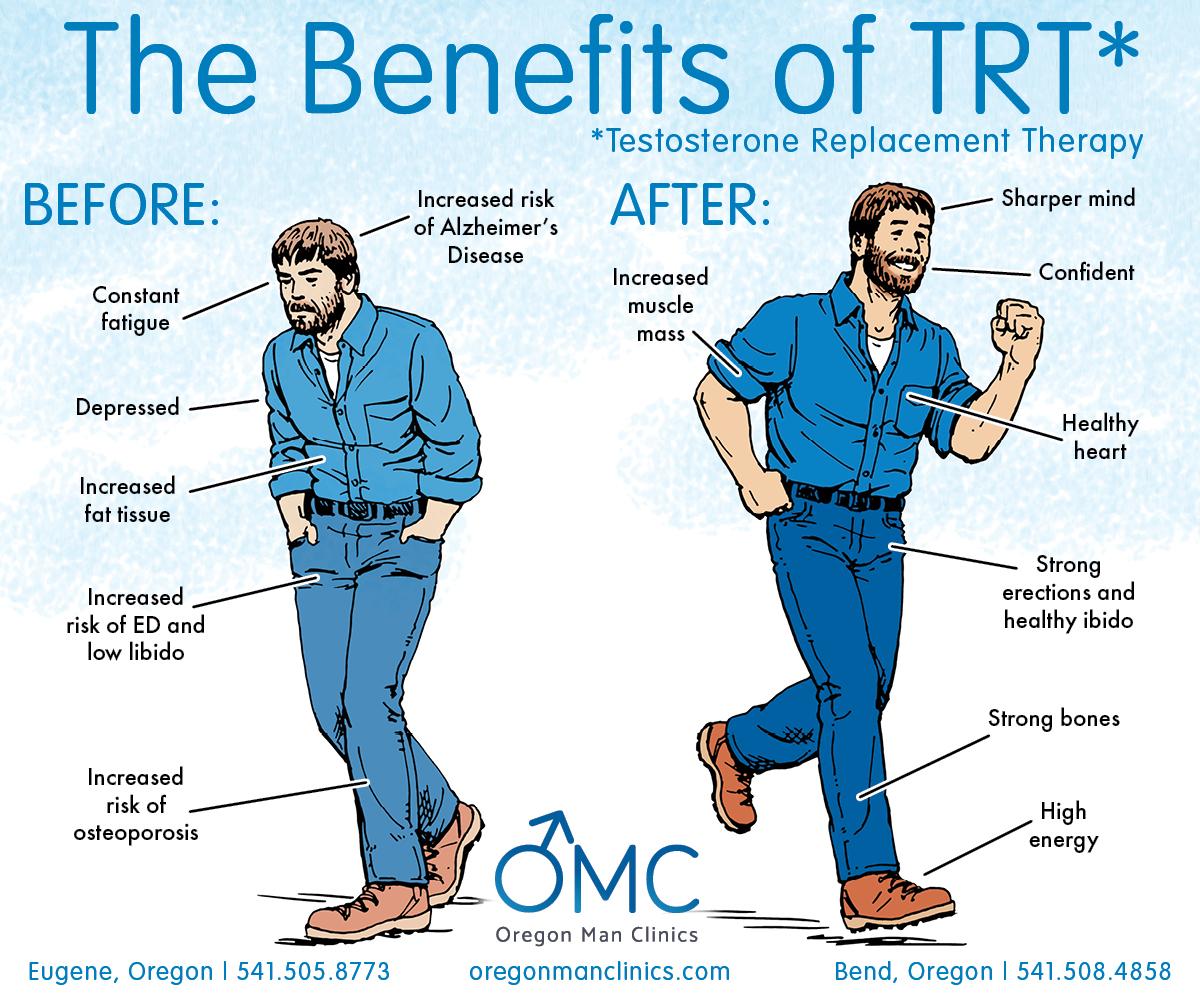
Navigating the Basics of Testosterone Therapy Dosage
Determining the appropriate dosage of testosterone therapy is a crucial step in ensuring both effectiveness and safety for individuals undergoing treatment. Recommendations may vary based on factors such as age, weight, overall health, and specific medical history. Therefore, it is essential for patients to engage in thorough discussions with their healthcare providers to tailor a regimen that meets their unique needs. Typically, the process begins with baseline testosterone level testing, followed by the introduction of therapy at an initial dosage that can be adjusted subsequently based on response and blood tests.
For many individuals, the typical starting dosage may range from 50 mg to 200 mg of testosterone, administered via injection, transdermal patches, or gels each week or bi-weekly. Regular follow-ups are critical to monitor physiological changes and side effects. A structured approach may include:
- Monitoring hormone levels: Blood tests every 3-6 months.
- Adjusting dosage: Incremental changes depending on testosterone levels and symptoms.
- Tracking side effects: Keeping a log of any adverse reactions.
| Administration Method | Typical Dosage |
|---|---|
| Intramuscular Injection | 50-200 mg weekly |
| Transdermal Patch | 2-6 mg daily |
| Topical Gel | 20-100 mg daily |
Understanding Individual Factors Influencing Dosage
Determining the appropriate dosage of testosterone therapy is not a one-size-fits-all approach; various individual factors play a critical role in tailoring treatment. Age, body composition, chronic health conditions, and lifestyle choices significantly influence how testosterone is metabolized and utilized in the body. For instance, older adults may experience a different response to therapy than younger individuals, often requiring adjustments in dosage. Similarly, those with higher body fat percentages might metabolize testosterone differently compared to those with leaner physique, impacting efficacy and side effects.
Moreover, genetics can dictate individual responses to hormone therapy. Different people may have varying levels of sensitivity to testosterone, which can affect how much of the hormone is needed to achieve optimal results. Comorbidities, such as diabetes or cardiovascular diseases, may also necessitate a more cautious approach, leading to lower dosages to avoid exacerbating existing health issues. Here’s a concise overview of these factors:
| Factor | Impact on Dosage |
|---|---|
| Age | Older adults may need lower doses |
| Body Composition | Higher body fat may require dosage adjustments |
| Genetics | Can affect sensitivity to testosterone |
| Chronic Health Conditions | May require cautious dosing and monitoring |
Assessing the Benefits of Accurate Testosterone Levels
Maintaining accurate testosterone levels is crucial for a myriad of physiological functions that ensure overall well-being. When testosterone levels fall within the optimal range, individuals may experience significant improvements in various aspects of their lives. Some of the notable benefits include:
- Enhanced energy levels: Balanced testosterone can lead to improved stamina and reduced fatigue.
- Improved mood and mental health: Adequate testosterone levels are linked to reduced symptoms of depression and anxiety, fostering a more positive outlook on life.
- Increased muscle mass and strength: Testosterone therapy can support muscle development, aiding in physical fitness and performance.
- Better libido and sexual function: Normal testosterone levels contribute to a healthy sex drive and improved sexual performance.
Furthermore, assessment of testosterone levels plays a critical role in personalizing treatment plans for those seeking therapy. Understanding the right dosage can empower healthcare providers to tailor interventions, leading to more effective outcomes. Consider the following table that illustrates the importance of proper dosage in relation to therapeutic goals:
| Goal | Dosage Range (mg/week) | Expected Benefit |
|---|---|---|
| Energy Enhancement | 50-100 | Increased vitality and reduced fatigue |
| Mood Improvement | 75-150 | Less anxiety and depressive symptoms |
| Muscle Building | 100-200 | Greater muscle mass and strength gains |
| Libido Boost | 75-125 | Enhanced sexual function and desire |

Monitoring and Adjusting Dosage for Optimal Outcomes
Monitoring testosterone therapy is crucial for achieving desired health outcomes. It is essential for both clinicians and patients to engage in ongoing dialogue about symptoms, side effects, and overall health status throughout the treatment process. Adjusting the dosage may be necessary based on various factors, including initial testosterone levels, response to therapy, and laboratory test results. Regular follow-ups and blood tests help in tailoring the dosage, ensuring that the therapy effectively restores hormone balance while minimizing potential risks. Patients should be encouraged to report any changes such as:
- Energy levels – both increases and decreases.
- Mood changes – including irritability or depression.
- Libido fluctuations – stable or unstable sexual desire.
Establishing an ideal dosage often follows a tailored approach, taking into account the individual’s health profile and lifestyle. The following table outlines initial dosing recommendations based on age and symptomatic presentation:
| Age Group | Initial Dosage (mg/week) | Adjustment Frequency |
|---|---|---|
| 18-30 | 50-100 | Every 6-8 weeks |
| 31-50 | 75-150 | Every 8-10 weeks |
| 51+ | 100-200 | Every 10-12 weeks |
As therapy progresses, periodic assessment is key to fine-tuning treatment. A patient’s metabolic response and blood work will guide necessary adjustments, which can differ widely among individuals. Keeping track of changes over time allows both the patient and healthcare provider to collaboratively reach the optimal therapeutic window, enhancing life quality and treatment efficacy.
Potential Risks and Side Effects of Testosterone Therapy
While testosterone therapy can offer various benefits, it is essential to be aware of the potential risks and side effects associated with its use. Some individuals may experience fluid retention, which can lead to swelling in the extremities or an increase in blood pressure. Additionally, there is a risk of developing acne or skin irritations as hormone levels fluctuate. A significant concern is the impact on cardiovascular health; some studies suggest a possible link between testosterone therapy and an increased risk of heart attacks or strokes. Furthermore, use of testosterone may affect the prostate, leading to potential complications such as benign prostatic hyperplasia (BPH) or prostate cancer in predisposed individuals.
Testosterone therapy may also bring about changes in mood and behavior, with some individuals experiencing aggressive behavior or mood swings. Sleep disorders, particularly sleep apnea, can be exacerbated by increased testosterone levels. In terms of metabolic effects, patients might face challenges such as higher cholesterol levels or elevated red blood cell count, which can increase the risk for clotting disorders. Given these risks, it is crucial for patients to undergo regular monitoring while on testosterone therapy, to help manage any developing side effects effectively. Below is a concise table summarizing common side effects:
| Side Effect | Potential Impact |
|---|---|
| Fluid Retention | Increased blood pressure and swelling |
| Acne/Skin Irritation | Discomfort and self-esteem issues |
| Cardiovascular Risks | Heart attacks, strokes |
| Mood Changes | Aggression, mood swings |
Guidelines for Ongoing Evaluation and Follow-Up
To ensure the effectiveness and safety of testosterone therapy, continuous monitoring is essential. Patients should undergo regular evaluations that may include:
- Lipid panel assessments to monitor cholesterol levels
- Hematocrit tests to check red blood cell counts
- Prostate-specific antigen (PSA) screenings to assess prostate health
- Standard hormone level tests to evaluate testosterone levels
Follow-up appointments should be scheduled every 3 to 6 months during the first year of therapy to determine the patient’s response and tolerance. As a guideline, consider implementing the following protocol for adjustments in therapy:
| Test Result | Recommended Action |
|---|---|
| Testosterone levels within normal range | No action needed; continue current dosage |
| Testosterone levels below normal | Increase dosage by 25-50mg |
| Testosterone levels above normal | Decrease dosage by 25-50mg |
| Hematocrit > 54% | Consider dose reduction or temporary discontinuation |
Emerging Trends and Research in Testosterone Dosage Practices
Recent studies in testosterone therapy have highlighted an increasing focus on personalized dosage strategies that cater to individual patient needs. Emerging research suggests that the traditional one-size-fits-all approach may not be the most effective, leading to a significant shift towards tailored treatments. Clinicians are now relying on a multifaceted assessment that includes serum testosterone levels, symptomatology, and patient preferences to devise optimal dosing regimens. Such personalization aims to enhance therapeutic outcomes, minimize side effects, and improve overall patient satisfaction.
The integration of technology into testosterone therapy is also gaining traction, with digital health tools enabling more precise monitoring of treatment efficacy and side effects in real-time. These tools can assist healthcare providers in adjusting dosages based on immediate feedback, further refining the therapeutic approach. Key aspects of this trend include:
- Continuous monitoring: Utilizing apps and wearable devices to track hormone levels and symptom changes.
- Data analytics: Leveraging data to identify patterns that inform dosage adjustments.
- Patient engagement: Empowering patients with information to participate in their treatment plans actively.
| Dosage Approach | Key Features | Benefits |
|---|---|---|
| Standardized Protocols | Fixed doses based on age/weight | Simple to implement |
| Personalized Strategies | Customized dosing based on individual response | Enhanced efficacy, reduced risk of adverse effects |
| Technology-Enhanced Dosing | Use of digital tools for real-time monitoring | Dynamic adjustments lead to better outcomes |
Q&A
Q&A: Understanding Testosterone Therapy Dosage Guidelines
Q1: What is testosterone therapy and who typically undergoes it?
A1: Testosterone therapy is a medical treatment aimed at restoring normal testosterone levels in men who have low hormone levels due to various reasons, including age, hypogonadism, or certain medical conditions. It’s also sometimes prescribed for women experiencing certain hormonal imbalances. The therapy seeks to alleviate symptoms such as fatigue, depression, and decreased libido, enhancing overall quality of life.
Q2: How is the appropriate dosage of testosterone determined?
A2: The appropriate dosage of testosterone is determined through a combination of blood tests, patient history, and clinical evaluation. Initially, physicians assess testosterone levels via blood tests, typically performed in the morning when testosterone levels are highest. Based on the results, doctors will consider factors such as age, weight, overall health, and specific symptoms when determining the dosage.
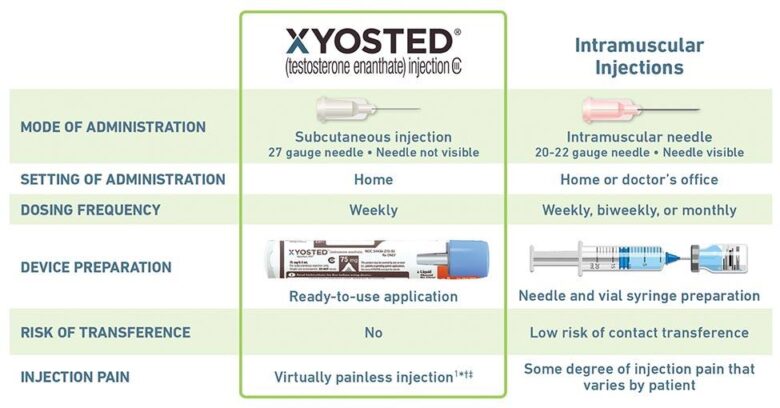
Q3: What are the common forms of testosterone therapy available?
A3: Testosterone therapy comes in several forms, including injections, transdermal patches, gels, pellets, and oral capsules. Each method has its own dosing schedule and duration. For clarity, for example, injections may be administered every one to two weeks, while gels are applied daily. The choice of form often depends on patient preference and specific therapeutic needs.
Q4: Are there standard dosage guidelines for testosterone therapy?
A4: While there are no one-size-fits-all dosage guidelines, a typical starting dose for testosterone replacement therapy may range from 50 mg to 200 mg per week for intramuscular injections, or 5 mg to 10 mg per day for transdermal applications. Physicians often start at the lower end of the range and adjust based on subsequent testosterone levels and patient response to treatment.
Q5: What factors can influence dosage adjustments during therapy?
A5: Several factors can necessitate dosage adjustments, including fluctuations in hormone levels as indicated by follow-up blood tests, side effects experienced by the patient, and the emergence of new symptoms. Lifestyle changes, such as weight gain or loss, and the onset of other health conditions can also impact how an individual metabolizes testosterone, thereby influencing dosage requirements.
Q6: What are the potential risks and side effects associated with testosterone therapy?
A6: Potential risks and side effects include acne, sleep apnea, increased red blood cell count, and an increased risk of heart disease or prostate issues. Because of these risks, regular monitoring with follow-up blood tests and health evaluations is essential throughout the course of therapy.
Q7: How often should patients on testosterone therapy have their levels checked?
A7: Patients undergoing testosterone therapy should typically have their testosterone levels monitored at regular intervals, usually every three to six months after starting therapy, then annually once stable levels are achieved. This helps ensure the therapy remains effective and side effects are managed promptly.
Q8: Is there a possibility of discontinuing therapy, and how is that approached?
A8: Yes, discontinuation of therapy is possible for various reasons, including the resolution of symptoms or the development of adverse side effects. If a patient and their doctor decide to stop therapy, it is usually done gradually, monitoring the patient’s natural testosterone levels as they adjust post-therapy. Patients should not discontinue without consulting their healthcare provider.
Q9: What should patients do if they have concerns about their testosterone therapy?
A9: Patients with concerns about their testosterone therapy should speak openly with their healthcare provider. Changes in mood, physical symptoms, or any side effects should be discussed, as these can guide adjustments to therapy. Open communication is key to optimizing treatment outcomes and ensuring patient safety.
Q10: Where can individuals find more information about testosterone therapy and its guidelines?
A10: Individuals can find comprehensive information from sources such as the Endocrine Society, the American Urological Association, and their healthcare providers, who can provide personalized insights based on individual medical histories. It is crucial to seek medically vetted information to make informed decisions about testosterone therapy.
The Way Forward
navigating the realm of testosterone therapy can be a complex journey, but understanding dosage guidelines is the first step towards unlocking the potential benefits of this treatment. As we’ve explored, individual considerations such as age, health status, and specific therapy goals play pivotal roles in determining the right dosage. It is essential for patients to engage in open dialogues with their healthcare providers, ensuring that personalization and safety remain at the forefront of their treatment plans. As research evolves and our understanding deepens, staying informed will empower you to make decisions that best support your health and well-being. Remember, the path to optimal hormonal balance is not one-size-fits-all – it’s a unique journey that deserves careful consideration and tailored guidance.