As the sun rises on our understanding of men’s health, a new chapter unfolds in the complex interplay of hormones and well-being. Testosterone, often celebrated for its role in vitality and strength, has recently stepped into the spotlight for another reason: its impact on prostate health. In an era where medical science continually reevaluates age-old beliefs, the conversation around testosterone therapy is both timely and necessary. This exploration delves into the nuances of testosterone therapy, examining its potential benefits and challenges for those navigating prostate health concerns. As we sift through the facts, myths, and emerging research, we aim to illuminate the path toward informed decisions that intersect with the delicate balance of hormones and health. Join us on this journey to uncover what testosterone therapy might mean for you or your loved ones in the quest for optimal prostate health.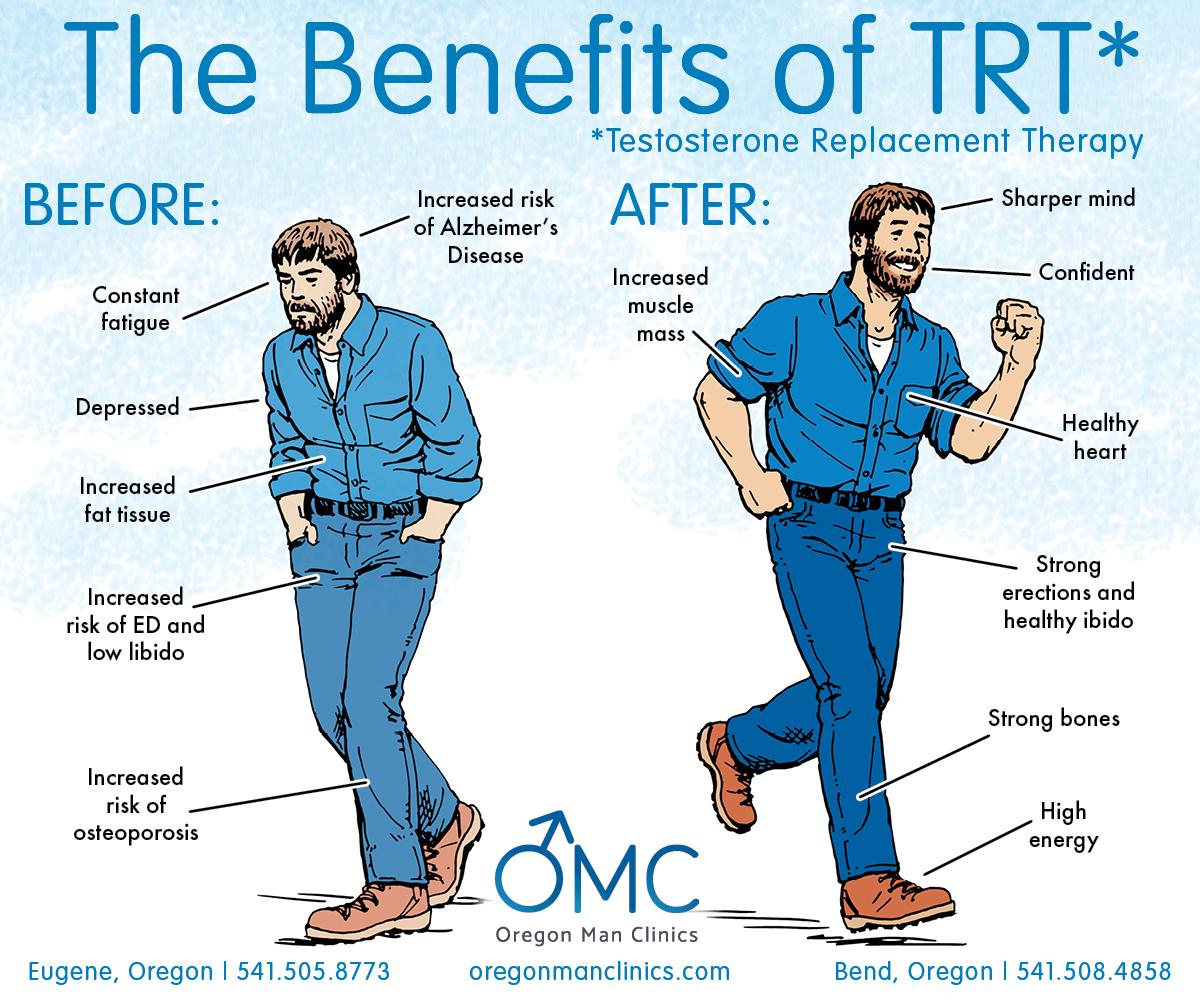
Understanding Testosterone Therapy and Its Role in Prostate Health
Testosterone therapy has emerged as a potential intervention for maintaining overall prostate health, especially in men who experience low testosterone levels. As men age, testosterone production naturally declines, leading to a range of health issues, including fatigue, depression, and even potential prostate complications. Undergoing testosterone therapy can help restore hormonal balance, which may play a crucial role in preventative prostate health measures. Men considering this treatment should be aware of the potential benefits and risks associated with testosterone reintroduction to the body.
When exploring the effects of testosterone therapy, it’s important to understand how this treatment interacts with prostate health. While some studies suggest that normal testosterone levels may actually be protective against prostate cancer, it’s essential to highlight that not all men are ideal candidates for therapy. Factors that may influence the appropriateness of testosterone treatment include:
- Existing prostate disorders: Men with a history of prostate cancer should approach therapy cautiously.
- Age: Older men may have different responses compared to younger individuals.
- Overall health: Pre-existing health conditions may require tailored approaches.
| Benefits of Testosterone Therapy | Considerations |
|---|---|
| Increases energy levels | Potential risk of prostate issues |
| Improves mood | Monitoring required for side effects |
| Enhances libido | Not recommended for all patients |
The Link Between Testosterone Levels and Prostate Function
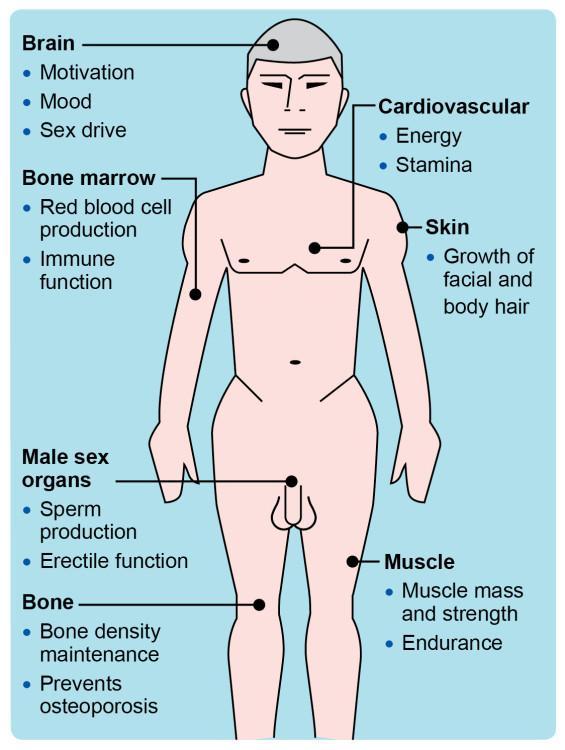
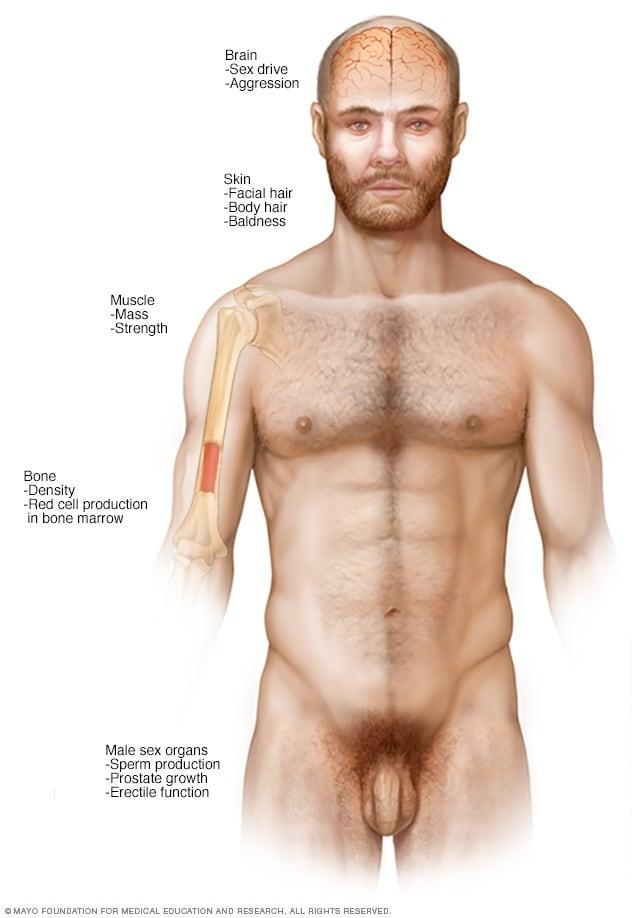
Understanding the relationship between testosterone levels and prostate function is essential for comprehending the implications of testosterone therapy on prostate health. Testosterone, a critical hormone in males, plays a key role in various bodily functions, including the maintenance of prostate tissue. Lower levels of testosterone can lead to changes in prostate size and function, which might result in benign prostatic hyperplasia (BPH) or even affect the health of the prostate in more complex ways. It is important to note that while testosterone contributes to prostate health, the impact of its supplementation can be multifaceted and requires careful management.
Research suggests several factors that detail how testosterone interacts with prostate function, including:
- Testosterone’s Role: It is essential for the development of prostate cells, influencing growth and maintenance.
- Balance is Key: Both low and high testosterone levels can contribute to prostate issues; moderation is crucial.
- Dihydrotestosterone (DHT): A potent derivative of testosterone that plays a significant role in prostate cellular processes.
| Testosterone Level | Prostate Health Impact |
|---|---|
| Low | May lead to BPH or other dysfunctions. |
| Normal | Supports healthy prostate functionality. |
| High | Potential risk for prostate cancer increase. |
The relationship between testosterone and prostate health is thus a delicate balance that necessitates a thorough understanding for anyone considering therapy. Monitoring hormone levels and understanding individual health profiles play a pivotal role in determining the appropriateness of testosterone therapy, ensuring that men can safely benefit from its potential advantages while minimizing risks. Future research continues to explore this intricate relationship to better guide treatment protocols and patient care.

Evaluating the Risks and Benefits of Testosterone Therapy
Testosterone therapy can offer various benefits for individuals looking to improve their overall health and well-being. Among these benefits are:
- Increased Muscle Mass: Testosterone plays a crucial role in muscle development, and therapy can help restore lean muscle.
- Enhanced Mood: Many patients report improved mood and a reduction in symptoms of depression and anxiety.
- Improved Bone Density: Higher testosterone levels can contribute to stronger bones, reducing the risk of fractures.
- Greater Libido: Individuals may experience enhanced sexual drive and function.
However, it is essential to weigh these benefits against the risks associated with testosterone therapy. Some potential concerns include:
- Prostate Health: Testosterone can stimulate prostate tissue, possibly increasing the risk of prostate-specific issues.
- Cardiovascular Risks: Some studies suggest that testosterone therapy may lead to an increased risk of heart-related conditions.
- Hormonal Imbalances: The therapy can disrupt natural hormone production, leading to side effects like infertility.
- Sleep Apnea: Testosterone therapy might exacerbate this condition, leading to serious health complications.
Clinical Guidelines for Safe and Effective Testosterone Treatment
The implementation of testosterone therapy necessitates adherence to stringent clinical guidelines to ensure both safety and efficacy, particularly concerning prostate health. Prior to initiating treatment, patients should undergo a comprehensive evaluation that includes serum testosterone levels, prostate-specific antigen (PSA) testing, and digital rectal examinations (DRE). This preliminary assessment is crucial for identifying any pre-existing conditions that may contraindicate therapy, such as prostate cancer or severe benign prostatic hyperplasia (BPH). Continuous monitoring through regular follow-ups is also essential, which typically involves:
- Monitoring testosterone levels (every 3-6 months initially)
- Assessing PSA levels annually
- Evaluating symptoms and side effects
In addition to screening and ongoing evaluations, the choice of administration method can significantly influence therapeutic outcomes. Options may include intramuscular injections, topical gels, or pellets, each with distinct profiles concerning efficacy and side effects. A recent review summarized these delivery methods as follows:
| Delivery Method | Frequency | Advantages | Disadvantages |
|---|---|---|---|
| Intramuscular Injections | Every 1-2 weeks | Quick absorption | Invasive, potential discomfort |
| Topical Gels | Daily | Non-invasive, easy application | Risk of transfer to others |
| Pellets | Every 3-6 months | Long-lasting | Requires minor surgical procedure |
Lifestyle Adjustments to Complement Testosterone Therapy
Integrating healthy lifestyle choices can significantly enhance the efficacy of testosterone therapy, amplifying its benefits for prostate health. Regular physical activity is crucial; engaging in both cardiovascular and strength-training exercises can optimize hormone levels while reducing the risk of prostate-related issues. Incorporating a balanced diet rich in nutrients helps support overall well-being. Focus on foods that are packed with antioxidants, particularly fruits and vegetables, as they can combat oxidative stress. Additionally, maintaining a healthy weight is key, as obesity can negatively influence testosterone levels.
Stress management also plays a vital role in maximizing the benefits of testosterone therapy. High levels of stress can lead to hormonal imbalances. Techniques such as meditation, yoga, or breathing exercises can help mitigate stress and promote hormonal health. Furthermore, ensuring adequate sleep quality is essential; aim for 7-9 hours each night to foster recovery and hormonal balance. Consider making adjustments such as establishing a regular sleep schedule, minimizing screen time before bed, and creating a restful sleeping environment. To encapsulate these adjustments, refer to the following table:
| Lifestyle Change | Benefit |
|---|---|
| Regular Exercise | Boosts testosterone levels & improves prostate health |
| Balanced Diet | Supports hormone function & reduces inflammation |
| Stress Management | Helps maintain hormonal balance |
| Quality Sleep | Promotes recovery & regulates hormone production |
Monitoring and Managing Potential Side Effects
When it comes to testosterone therapy, careful observation is paramount to ensure the well-being of individuals seeking treatment for prostate health. Patients should be encouraged to maintain open communication with their healthcare providers regarding any changes in their health status. Regular check-ups allow for the timely identification of potential side effects, which may include:
- Gynaecomastia: Breast tissue enlargement that may require intervention.
- Fluid Retention: Swelling in the legs or feet, indicating changes in body fluid balance.
- Sleep Apnea: A condition that can exacerbate during testosterone therapy, affecting sleep quality.
- Increased Hematocrit: Elevated red blood cell count which may increase the risk of cardiovascular events.
Monitoring strategies should include blood tests and assessments of prostate-specific antigen (PSA) levels, ensuring that any abnormalities are addressed promptly. Patients should also be educated about recognizing symptoms that require immediate medical attention, such as chest pain or severe headaches. Below is a summary of key monitoring strategies:
| Monitoring Aspect | Frequency | Notes |
|---|---|---|
| PSA Levels | Every 3-6 months | To identify any suspicious changes. |
| Complete Blood Count | Every 6-12 months | To monitor red blood cell levels and hematocrit. |
| Liver Function Tests | Annually | To ensure liver health is maintained. |
Future Directions in Research on Testosterone and Prostate Health
As the landscape of testosterone therapy continues to evolve, future research will be pivotal in uncovering the nuanced relationship between testosterone levels and prostate health. Emerging studies are increasingly focusing on the duality of testosterone’s effects, aiming to unravel the complexities that underpin its role in both promoting health and the potential risks associated with therapy. Key areas for investigation include:
- Longitudinal Studies: Conducting extensive, multi-year studies to track the impact of testosterone therapy on prostate health across diverse populations.
- Biomarker Identification: Exploring potential biomarkers that could predict the effects of testosterone therapy on individual patients.
- Dosage Optimization: Determining the optimal dosage and administration methods for testosterone therapy to maximize benefits while minimizing risks.
Furthermore, the interaction between lifestyle factors and testosterone levels presents another fertile area for exploration. This includes examining how diet, exercise, and mental health influence testosterone’s impact on prostate health. Future research may also delve into:
- Genetic Factors: Investigating the genetic predispositions that may influence individual responses to testosterone therapy.
- Comparative Studies: Assessing the differences in outcomes between various testosterone formulations to better guide clinical practice.
- Patient-Reported Outcomes: Focusing on the subjective experiences of patients undergoing testosterone therapy to understand quality of life improvements alongside potential health risks.
Q&A
Q&A: Testosterone Therapy for Prostate Health
Q1: What is testosterone therapy, and how does it relate to prostate health?
A1: Testosterone therapy involves the administration of testosterone to men who have low levels of this hormone, often due to age or medical conditions. While testosterone is critical for various bodily functions, its relationship with prostate health is complex. Some studies suggest that testosterone therapy may not directly increase the risk of prostate cancer, while others highlight the importance of monitoring prostate health in individuals undergoing treatment.
Q2: Who should consider testosterone therapy?
A2: Testosterone therapy may be considered for men exhibiting symptoms of testosterone deficiency, such as fatigue, reduced libido, and decreased muscle mass. However, it is essential to consult a healthcare provider who can assess individual health status and determine whether the potential benefits of therapy outweigh the risks, especially regarding prostate health.
Q3: Are there any risks associated with testosterone therapy concerning prostate health?
A3: Yes, there are potential risks associated with testosterone therapy. Some studies have raised concerns that it could stimulate the growth of existing prostate cancer or benign prostate hyperplasia (BPH). Therefore, men with a history of prostate cancer or those at high risk should engage in thorough discussions with their healthcare providers before starting therapy.
Q4: How can I monitor my prostate health while on testosterone therapy?
A4: Regular monitoring is crucial for maintaining prostate health during testosterone therapy. This typically includes periodic prostate-specific antigen (PSA) blood tests, digital rectal exams (DRE), and an overall assessment of urinary symptoms. Staying in close communication with your healthcare provider can help ensure any changes are caught early.
Q5: Is there a connection between testosterone levels and prostate cancer risk?
A5: The connection between testosterone levels and prostate cancer risk remains a topic of debate in the medical community. Some research suggests that high testosterone levels might be linked to an increased risk of prostate cancer, while other studies indicate that low levels could also have negative effects. This intricate relationship calls for a personalized approach to treatment and monitoring.
Q6: Are there alternatives to testosterone therapy for managing low testosterone symptoms?
A6: Yes, there are alternatives to testosterone therapy. Lifestyle changes such as regular exercise, a healthy diet, stress management, and getting adequate sleep can help manage low testosterone symptoms. Furthermore, some medications and supplements may assist in improving testosterone levels or mitigating symptoms without the associated risks of hormone therapy.
Q7: What should I discuss with my healthcare provider before starting testosterone therapy?
A7: Before starting testosterone therapy, it’s essential to discuss your complete medical history, any pre-existing prostate issues, potential side effects, and your specific health goals. Additionally, inquire about the monitoring plan and any lifestyle modifications that could enhance therapy’s effectiveness and mitigate risks.
Q8: what is the key takeaway regarding testosterone therapy and prostate health?
A8: The key takeaway is that testosterone therapy can have benefits for men with low testosterone, but it comes with potential risks, particularly concerning prostate health. A balanced approach that includes thorough medical evaluations, regular monitoring, and open communication with healthcare providers is essential for managing treatment effectively and safely.
To Conclude
the exploration of testosterone therapy for prostate health opens up a complex yet intriguing dialogue about the balance between hormone levels and overall wellness. As research continues to unveil the nuances of testosterone’s role within the male body, it becomes increasingly clear that this therapy is not a one-size-fits-all solution. Individual considerations, such as age, health status, and personal risk factors, must guide any decision regarding testosterone supplementation.
With the potential to enhance quality of life and address specific health concerns, testosterone therapy can be a valuable tool in the right hands. However, it’s essential for individuals to engage in thorough discussions with their healthcare providers, fostering an informed pathway that prioritizes safety and efficacy.
Ultimately, as we recalibrate our understanding of hormones and their impact on prostate health, we step into a future where personalized medicine paves the way for empowered choices and better health outcomes. Navigating this realm with careful consideration will ensure that we embrace not just the advancements in therapy, but also the age-old wisdom of holistic well-being.










