In the intricate tapestry of human biology, hormones play pivotal roles in shaping not only our physical form but also our very essence of vitality and reproduction. Among these chemical messengers, testosterone stands out as a key player in male fertility, influencing everything from libido to sperm production. Yet, in an era where the pressures of modern life often lead to hormonal imbalances, the quest for viable solutions brings us to the forefront of a significant medical discussion: testosterone therapy. This article delves into the nuances of testosterone therapy for male fertility, exploring how this treatment may serve as a beacon of hope for those navigating the challenges of conception, the science underpinning its efficacy, and the considerations that must be weighed before embarking on this therapeutic journey. As we unravel the complexities of male reproductive health, we aim to shed light on the potential benefits and risks associated with testosterone therapy, empowering men and their partners to make informed decisions about their fertility and future.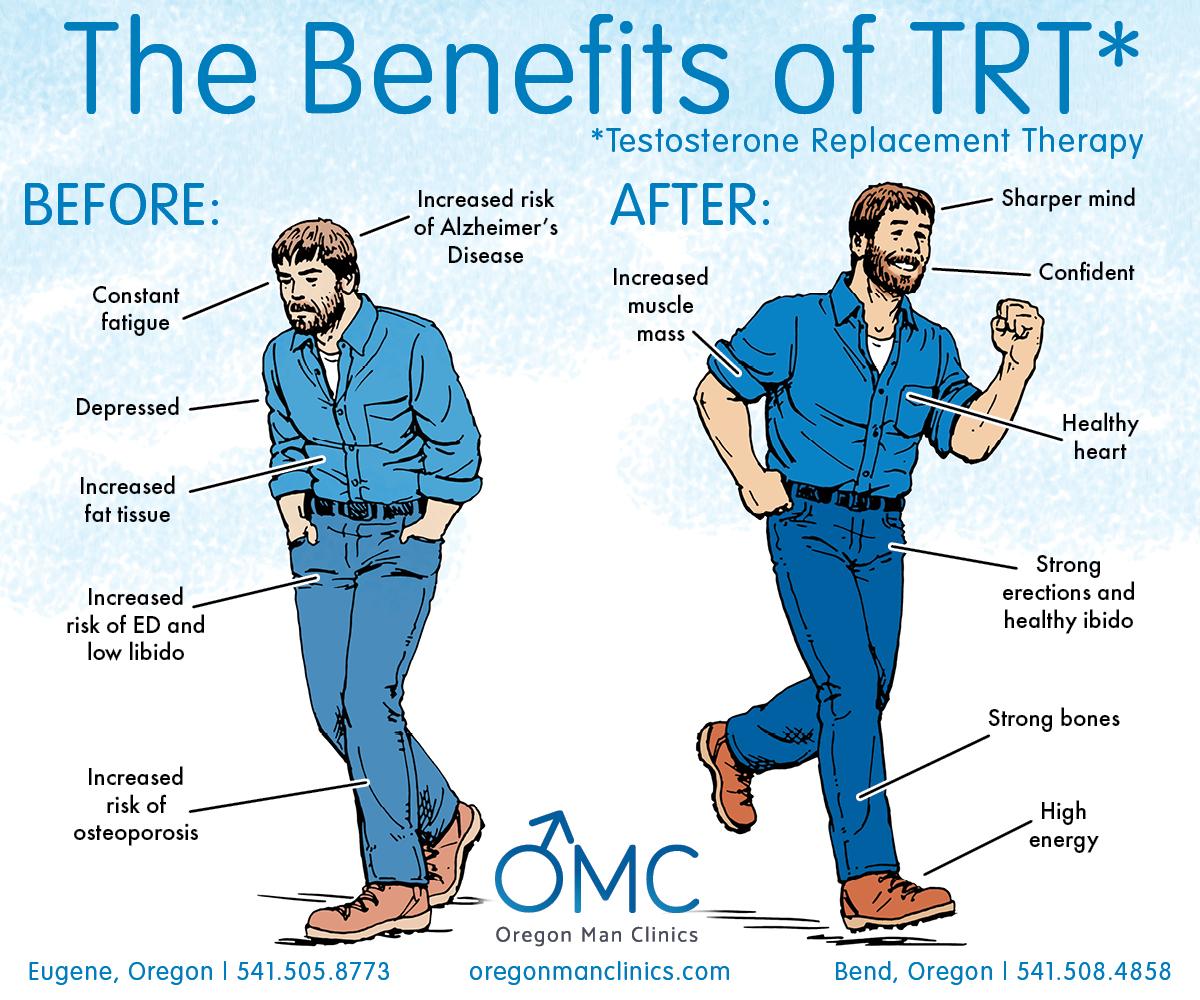
Understanding the Role of Testosterone in Male Fertility
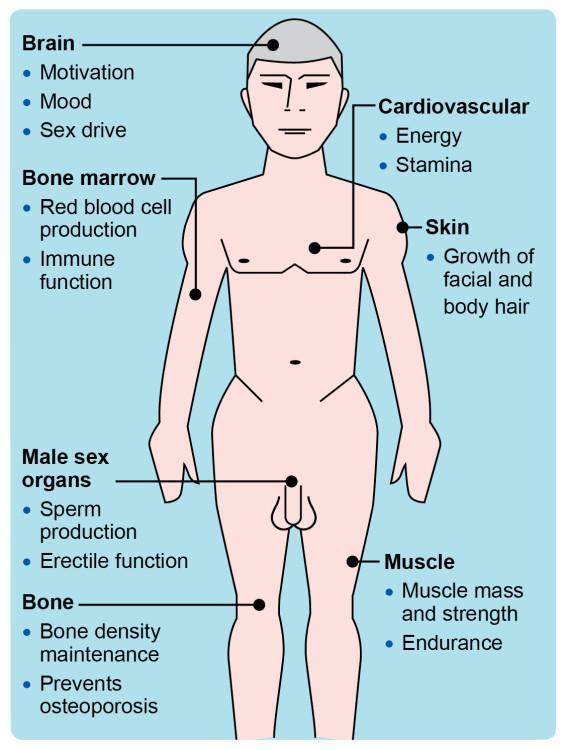
Testosterone plays a crucial role in various aspects of male fertility, influencing not only libido but also the production and maturation of sperm. Adequate levels of testosterone are essential for maintaining spermatogenesis, the process through which sperm cells are generated. When testosterone levels drop, men can experience fertilization issues, as low testosterone is often associated with decreased sperm quality and quantity. Supporting overall reproductive health requires a delicate balance, as both low and excessively high levels of testosterone can negatively impact fertility.
Testosterone therapy has emerged as a potential treatment for those struggling with infertility linked to low hormonal levels. Individuals considering this therapy should be evaluative of the benefits and risks involved. Some key considerations include:
- Individual evaluation: Each man’s hormonal profile is unique; therefore, personalized assessments are essential.
- Side effects: Possible implications of therapy may include mood changes, acne, or increased risk of sleep apnea.
- Impact on sperm production: Therapy may temporarily affect sperm production and should be monitored by a healthcare professional.
For those actively exploring testosterone therapy, it’s important to engage with specialists who can provide evidence-based insights and tailored approaches. Understanding how testosterone interplays with the intricate process of male fertility can empower men to make informed decisions regarding their reproductive health.
Exploring the Benefits and Risks of Testosterone Therapy
Testosterone therapy presents a range of potential benefits for men seeking to enhance their fertility. By elevating testosterone levels, men may experience improved libido, increased spermatogenesis, and enhanced overall reproductive health. This therapy could be particularly beneficial for those dealing with low testosterone, often characterized by symptoms such as fatigue, decreased muscle mass, and mood fluctuations. Here are some identified benefits:
- Enhanced Sexual Function: Quality and frequency of sexual activity may improve.
- Increased Energy Levels: Higher testosterone levels can lead to greater physical vitality.
- Improved Mood: Many patients report enhanced mood stability and reduced depressive symptoms.
However, alongside the potential benefits, it is crucial to recognize the associated risks of testosterone therapy. This treatment is not without its complications, and understanding these can aid in making informed decisions. Some of the concerns include the possibility of infertility, blood clots, and prostate health issues. Here are some risks to consider:
- Testosterone Suppression: Therapy can lead to decreased natural testosterone production.
- Cardiovascular Issues: An increased risk of heart attacks or strokes has been observed.
- Potential Hormonal Imbalance: May cause elevations in estrogen levels, leading to side effects.

Recognizing Symptoms of Low Testosterone Levels
Identifying low testosterone levels is crucial for maintaining overall male health, especially when considering its impact on fertility. Common signs that may indicate a deficiency include:
- Reduced libido: A noticeable decline in sexual interest or arousal.
- Erectile dysfunction: Difficulty achieving or maintaining an erection.
- Fatigue: Unexplained tiredness or a decrease in energy levels, affecting daily life.
- Muscle mass loss: Decreased muscle strength or volume, even with regular exercise.
- Mood changes: Increased irritability, depression, or difficulty concentrating.
In addition to these symptoms, certain physical changes may also signal low testosterone. Men might witness:
| Physical Change | Description |
|---|---|
| Weight gain: | Accumulation of body fat, particularly around the abdomen. |
| Changes in hair growth: | Thinning hair on the head or decreased body hair. |
| Hot flashes: | Sudden feelings of warmth, often accompanied by sweating. |
Recognizing these signs early can lead to timely assessment and intervention, paving the way for the appropriate management of low testosterone levels, particularly as it relates to fertility and reproductive health.
Evaluating the Impact of Testosterone Therapy on Sperm Production
Testosterone therapy has gained significant attention as a potential solution for various hormonal deficiencies and related health concerns among men. However, when considering its application in the context of male fertility, the challenge lies in understanding how increased testosterone levels may influence sperm production. While testosterone is vital for the development of male reproductive tissues and the production of sperm, exogenous testosterone administration often leads to a physiological response that can result in suppression of spermatogenesis. This paradox invites a closer examination of how elevated testosterone levels can coincide with changes in sperm quality and count.
Research indicates that while testosterone therapy can improve libido and overall well-being, it may also yield a decrease in sperm output. The effects of therapy can vary significantly based on dosage and duration of treatment. Key factors to consider include:
- Dose dependency: Higher doses of testosterone can lead to greater suppression of sperm production.
- Duration of therapy: Prolonged use tends to exacerbate negative outcomes on fertility.
- Individual variability: Responses to therapy can differ widely based on genetic and environmental influences.
To provide an overview, the following table illustrates some potential outcomes of testosterone therapy on sperm parameters:
| Parameter | Effect of Testosterone Therapy |
|---|---|
| Sperm Count | May decrease |
| Sperm Motility | Potential reduction |
| Sperm Morphology | Might remain unchanged |
Ultimately, the interplay between testosterone therapy and sperm production necessitates a nuanced approach, emphasizing the importance of personalized treatment strategies that consider the individual’s reproductive goals alongside hormone optimization.
Best Practices for Monitoring and Adjusting Testosterone Treatment
Effective monitoring and adjustment of testosterone treatment are crucial in optimizing male fertility outcomes. Regular follow-ups with healthcare professionals should include hormonal level assessments, symptom evaluations, and side effect monitoring. It’s essential to maintain a dialogue about any changes noticed during treatment, whether positive or negative, as this feedback can guide dosage adjustments. Comprehensive management should also encompass lifestyle factors that may influence testosterone levels, such as diet, exercise, and sleep quality, empowering patients to take an active role in their fertility journey.
To structure an efficient monitoring plan, consider tracking the following key metrics:
- Serum Testosterone Levels: Measured typically every 3-6 months.
- SHBG and Free Testosterone: Important for understanding hormonal balance.
- Semen Analysis: Conducted to assess fertility potential before and during treatment.
- Side Effects: Document any adverse effects for timely intervention.
| Metric | Frequency | Purpose |
|---|---|---|
| Serum Testosterone Levels | Every 3-6 months | Assess treatment effectiveness |
| SHBG and Free Testosterone | Annual | Understand hormonal balance |
| Semen Analysis | Every 6 months | Evaluate fertility potential |
| Side Effects Check | At every appointment | Monitor patient comfort |
Lifestyle Changes to Complement Testosterone Therapy
To maximize the benefits of testosterone therapy, integrating lifestyle modifications is essential. These holistic adjustments can support hormonal balance and enhance overall well-being. Consider adopting the following practices:
- Balanced Diet: Emphasize whole foods with a focus on lean proteins, healthy fats, and an abundance of fruits and vegetables. Nutrient-rich diets can boost energy levels and support hormonal health.
- Regular Exercise: Engaging in both strength training and cardiovascular workouts can significantly improve testosterone levels. Aim for a combination of resistance training and aerobic activities at least three times a week.
- Sufficient Sleep: Prioritize 7-9 hours of quality sleep each night. Sleep is crucial for the body’s recovery processes and hormonal regulation.
- Stress Management: Incorporate mindfulness techniques such as meditation, yoga, or deep-breathing exercises to lower cortisol levels, which can negatively impact testosterone.
Furthermore, habits such as quitting smoking and reducing alcohol consumption can lead to dramatic improvements. Here’s a brief overview of how certain lifestyle changes relate to testosterone levels:
| Change | Impact on Testosterone |
|---|---|
| Regular Exercise | Increases levels |
| Low Sugar Intake | Helps maintain balance |
| Stress Management | Reduces negative effects |
| Adequate Sleep | Supports production |
By implementing these changes alongside testosterone therapy, individuals can create a synergistic effect, promoting fertility, vitality, and overall health.
Consulting Healthcare Professionals: Navigating Your Fertility Journey
When embarking on your fertility journey, consulting with healthcare professionals is essential to making informed decisions about testosterone therapy and its impact on male fertility. Testosterone levels can influence various aspects of reproductive health, from sperm production to libido. Before starting therapy, a thorough evaluation is crucial, including comprehensive hormonal testing and an assessment of any underlying health issues that may contribute to fertility struggles. A tailored approach, guided by specialists in endocrinology or urology, ensures that testosterone therapy addresses individual needs without compromising reproductive potential.
During your consultation, it’s important to discuss the following factors:
- Potential side effects of testosterone therapy, such as decreased sperm production and testicular atrophy.
- Alternative treatments that might be more suitable, like clomiphene citrate or human chorionic gonadotropin (hCG).
- Lifestyle modifications that can enhance fertility, such as diet, exercise, and stress management.
- Monitoring plans for tracking testosterone levels and fertility parameters throughout the treatment process.
Your healthcare provider should also provide a comprehensive overview of how therapy may affect your overall health, helping you to navigate this complex landscape with confidence.
Q&A
Q&A: Understanding Testosterone Therapy for Male Fertility
Q1: What is testosterone therapy, and why is it considered for male fertility?
A1: Testosterone therapy involves administering testosterone to men who have low levels of the hormone, which can negatively impact various bodily functions, including fertility. Low testosterone, or hypogonadism, may lead to decreased sperm production, affecting a man’s ability to conceive. Therapy aims to restore hormonal levels to improve overall reproductive health.
Q2: How does testosterone impact male fertility specifically?
A2: Testosterone plays a crucial role in the male reproductive system. It is involved in the production of sperm within the testicles. When testosterone levels are low, spermatogenesis (the process of sperm production) can be impaired, leading to reduced sperm count and quality. Conversely, we must be cautious, as supplementing testosterone can also suppress natural production and ultimately lower sperm count if not managed properly.
Q3: Who is a candidate for testosterone therapy in relation to fertility issues?
A3: Candidates typically include men diagnosed with low testosterone levels who are experiencing infertility. However, it is essential to conduct a thorough assessment by a healthcare provider, as not all men with low testosterone face fertility challenges. Doctors will evaluate hormone levels, symptoms, and overall health to determine if testosterone therapy is appropriate.
Q4: Can testosterone therapy help improve fertility outcomes?
A4: It can, but the effects vary among individuals. In some cases, restoring testosterone levels may enhance sperm production and improve fertility. However, in others, testosterone therapy can suppress natural testosterone and sperm production. Therefore, it’s often best to explore alternative treatments like human chorionic gonadotropin (hCG) or Clomiphene citrate, which can stimulate natural testosterone production without impacting fertility.
Q5: What are the potential risks associated with testosterone therapy?
A5: As with any medical treatment, there are potential risks. Testosterone therapy can lead to side effects such as sleep apnea, increased red blood cell count, and mood swings. In some cases, it may also increase the risk of cardiovascular issues. It’s essential to discuss these risks with a healthcare professional before starting therapy and to monitor health throughout the treatment.
Q6: Are there natural ways to boost testosterone without therapy?
A6: Yes, several lifestyle changes can naturally increase testosterone levels. These include maintaining a balanced diet rich in healthy fats, regular exercise, managing stress, and ensuring adequate sleep. Avoiding substance abuse, such as excessive alcohol or drugs, can also support healthier testosterone production. Additionally, addressing underlying health issues like obesity or diabetes may lead to improvements in hormonal balance.
Q7: What should men consider before starting testosterone therapy for fertility?
A7: It’s vital for men to have an open discussion with their healthcare provider about their specific fertility concerns and the potential benefits and drawbacks of testosterone therapy. Comprehensive testing should be conducted, including hormone levels and sperm analysis. Men should also consider alternative strategies that could address underlying issues without the need for therapy and weigh the importance of achieving both hormonal balance and healthy sperm production.
Q8: Can men with restored testosterone levels still face fertility challenges?
A8: Yes, restoring testosterone levels does not guarantee fertility. Factors like age, additional medical conditions, and genetic predispositions can still play a significant role in male fertility. For men seeking to conceive, it’s essential to work closely with a fertility specialist who can provide personalized guidance and treatment options tailored to individual needs.
Q9: What is the takeaway for men considering testosterone therapy for fertility?
A9: The decision to pursue testosterone therapy for enhancing fertility should be made cautiously and ideally in conjunction with a healthcare provider. Understanding the nuances of how testosterone affects fertility and exploring a holistic approach to reproductive health can lead to more informed choices and potentially better outcomes. Remember, every path is unique, and a strategy tailored to individual circumstances can make all the difference.
In Summary
the landscape of male fertility is evolving, and testosterone therapy stands at the forefront of this change. While the promise of hormonal treatment offers hope for those facing fertility challenges, it’s essential to tread carefully. The intricate balance of hormones and the multifaceted nature of reproductive health demand a nuanced approach, grounded in both medical expertise and personal insight. As research continues to unfold, the conversation around testosterone therapy will likely expand, inviting further scrutiny and understanding. For men considering this path, collaboration with healthcare professionals is crucial to navigating the potential benefits and risks. Ultimately, the journey towards becoming a father is as unique as each individual, and equipped with the right knowledge and support, it can lead to fulfilling outcomes, both in the realm of fertility and beyond.










